Protective equipment for physicians' mental health
The Emotional PPE Project is a nonprofit directory that connects health care workers with licensed mental health professionals, which has become particularly important during the COVID-19 pandemic.
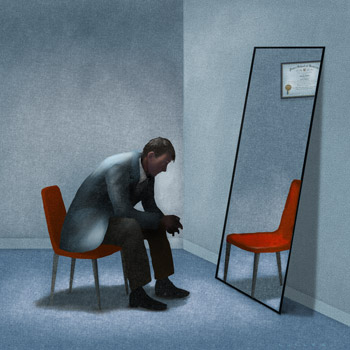
For many physicians, the prospect of talking about their own mental health problems carries the same warning as an arrest: You have the right to remain silent, and anything you say can and will be used against you.
Medical licensing applications, for example, can include questions addressing the mental health of applicants, although that's beginning to change. In 2018, the Federation of State Medical Boards (FSMB) adopted a policy recommending that state boards approach physician wellness and burnout from a nonpunitive perspective, evaluating whether it is necessary to ask probing questions about mental health, addiction, or substance use, particularly in the applicant's past.

While not all state medical board questions adhere to FSMB recommendations yet, they have moved in that direction, according to a study published as a research letter in May by JAMA. Thirty-nine states limited questions on initial licensing applications to current conditions with impairment, a nearly twofold increase from the 21 states in a 2017 study published in Mayo Clinic Proceedings.
But with the recommendations still not fully adopted, many physicians likely remain reluctant to seek help for mental health conditions. This is especially concerning during the COVID-19 pandemic, which has greatly increased clinicians' mental health care needs, said Eileen Barrett, MD, MPH, MACP, who coauthored the JAMA study and is an associate professor at the University of New Mexico School of Medicine in Albuquerque and a former ACP Regent and Governor.
Dr. Barrett, who is also an ACP Well-being Champion, and coauthors Ariel Brown, PhD, a Massachusetts-based psychiatry and neurology researcher, and Daniel Saddawi-Konefka, MD, MBA, program director of the anesthesia residency at Massachusetts General Hospital in Boston, recently joined ACP Internist for a conversation about physician mental health and COVID-19. At the start of the pandemic, Drs. Brown and Saddawi-Konefka cofounded the Emotional PPE Project, a nonprofit directory that connects health care workers with licensed mental health professionals.
Q: What's wrong with medical licensing application questions about physicians' mental health?
A: Dr. Barrett: Many of these questions violate the Americans with Disabilities Act. The other thing is the human part … these questions perpetuate the stigma about receiving mental health care or having a mental health diagnosis, resulting in physicians not receiving care. Additionally, a study in the Journal of Psychiatry showed that oftentimes, these questions aren't answered accurately. And the reason, of course, is because there is bias and discrimination toward physicians as a result of having mental health diagnoses. These questions can also falsely equate having a mental health diagnosis with providing inferior care. When asking these questions and penalizing physicians for seeking treatment, we are not doing the difficult and the deep work that needs to be done to ensure patient safety.
Dr. Brown: Does the intention of these questions actually result in better-quality care? Does it actually result in better patient safety? Or does it actually result in more impaired physicians because of the deterrents [to seeking help] being there? It's very hard for me to understand at this point, with what we know about mental health and what we know about the stressors of training and of being a physician right now, why we would want any barriers to getting some support.
Q: How has the COVID-19 pandemic increased clinicians' mental health needs?
A: Dr. Barrett: A small number of physicians have taken care of their own colleagues who have been hospitalized and who may have died from COVID-19. That's incredibly traumatizing for them—especially if it happened when there was not enough PPE [personal protective equipment], when there was deliberate disinformation about COVID-19, and also rationing of PPE. And for a lot of the health care workers who became infected with COVID, they felt shame—and I wish that that weren't the case.
Dr. Saddawi-Konefka: We see people on their absolute worst days, and oftentimes this happens, and then the next case is coming in, and you've just got to move on. … It's hard to see all that trauma, day in and day out, and then heading into a pandemic, which is not something that people knew they had signed up for.
Dr. Brown: What happens to all those experiences and those feelings when you're in a system that punishes you for talking about that you need support? That's, I think, where we're hoping the Emotional PPE Project will come in. … Supports are out there, and we want to encourage people to use them so that they can feel better, so that they can perform better, so that they can re-enter into whatever level of normalcy might come next.
Q: How did the Emotional PPE Project get started?
A: Dr. Brown: Last spring, when we started to put together this program, we said, “All right, we know that these folks are under undue, unprecedented levels of stress. We want to basically make it easy for people who are supposed to be these heroes and lifting us up out of the pandemic to get the support that they need.” We didn't actually have a lot of insight into the barriers at that point; we just wanted to help, at first, [Dr. Saddawi-Konefka's] residents—and then physicians, nurses, and other health care workers as the problem became clear to us that people really need a lot of support and are not getting it.
Dr. Saddawi-Konefka: The first seedlings of the project were … a directory of volunteer therapists across the country who all wanted to help. And the project itself, we collect no information about any of the users. In other words, all of the contact is done directly between the health care worker and the psychiatrist or therapist.
Q: How can the Emotional PPE Project and similar organizations help physicians?
A: Dr. Brown: We assume there's a population of people that want to talk to a professional, and what has been advertised to them is actually through their employment institution. The [employee assistance programs] are popular amongst hospital administration; they're not particularly popular amongst users because when you are living in this cloud of stigma, you don't want to be raising your hand to somebody that's connected to your HR department. So the benefit of Emotional PPE Project directory and similar organizations that are out there is … the confidentiality piece.
When you see a therapist and the therapist bills the insurance company, they actually have to give you a diagnosis. The insurance company will not pay for your therapy session unless you have a diagnosis. Emotional PPE Project does not take any money and does not take any insurance, so it is literally one person who needs some help and a volunteer, professional mental health clinician that wants to give it for free, not connected to a client institute, and not billing any insurance company that's going to require a diagnosis. We have had about 1,000 people use our service so far over the past year.
Dr. Saddawi-Konefka: We do ask the therapists to tell us if they got used and what type of health care worker it was, but we don't collect any [personal data]. It's free, it's confidential, the therapists are typically willing to meet you whenever you need. There's availability if you can only meet in the evenings or weekends.
Q: What is your advice for physicians who are dealing with mental health problems or who want to support their colleagues in getting help?
A: Dr. Saddawi-Konefka: Health care workers are, sadly, notorious for not taking adequate care of themselves. We overlook subtle symptoms. For me, my symptoms were I just felt more irritable with my kids. I was also a little more tired. But we think, “Oh, it's probably normal. I don't need to do anything,” and keep working. This is the same cohort of people who, in order to come into work, we had to do COVID symptom screens because we just ignore our symptoms, and I think we do it with mental health as well. Often, health care workers really only seek help when they're close to a breaking point or really on the cusp of so burnt out, the rope is about to snap. And there's just no reason to wait that long. … If you feel 85% of normal, you don't have to persist with that. You deserve that 15%. That tends to be the 15% that you spend at home with your family or on yourself.
Pay attention to how you're feeling, and really take a chance on getting help. Especially if you go through programs like Emotional PPE that are free and don't collect any information about users, there's really nothing to lose. … The second piece of advice is to advocate for your colleagues. And I've noticed this, certainly, as a program director. There are so many residents who clearly would benefit from talking to someone, and they know it, and they know how easy it is. But they don't do it until they get a little bit of prodding and a check-in like, “So did you actually reach out?”
Dr. Brown: Telling your own story really helps others as well, so [try] showing a little bit of vulnerability to your colleagues. If you have, for instance, in the past seen a therapist or in the past reached out to a professional for some support, people who are respected who say that, it really makes a difference in other people's lives.
Dr. Barrett: No matter what you feel, you are not alone. … If you think you work someplace where experiencing a mental health stressor or crisis is not an issue, it means that you're mistaken. And that's not your fault; it's because people are hiding it, and they're hiding it for lots of reasons. They're hiding it because of the cultural and structural barriers to receiving mental health care, and also the cultural and structural barriers to having good mental health. We have many mentally unhealthy workplaces. But here's something important: The cultural and structural barriers are a choice. And we can choose something different.
I hope that everybody who reads this article, that the first thing that they do is work to change their credentialing applications to not ask about mental health. That could be as easy as an email to your medical staff office or to human resources asking them to remove questions that stigmatize mental health care. The second step is to be proactive about sharing mental health resources, such as Emotional PPE, also the Physician Support Line, any state-based resources, and also any employee assistance programs. Third, add those mental health resources as contacts to your phone so that then you can share them with others. And, last, host a grand rounds on this topic, because that's how we start to change the culture.
Q: Looking forward, do you foresee improvements in the culture around physician mental health?
A: Dr. Brown: Yes. I think we've made so much progress so far, from 10 years ago, from five years ago, from one year ago. And I think as long as we keep doing this work and people keep coming forward as champions, then there is a lot of progress that's going to be made.
Dr. Saddawi-Konefka: Listening to my residents now versus even my residents five, 10 years ago, people talk about this. They didn't used to talk about this. And I know that these are who are going to be leading health care in the future.
Dr. Barrett: We even see [change] in ACP … There's also an entire resource hub and a whole series of Well-being Champions. ... So I really think that we'll get there, and we'll get there because it's the right thing to do.