MKSAP Quiz: 12-hour history of fever
A 51-year-old man is evaluated in the emergency department for a 12-hour history of fever, chills, headache, and weakness. He works on his farm in Maine and spends a considerable part of most days outside, but he is not aware of any tick or mosquito bites. He has had no diarrhea, cough, or rash. The patient had his spleen surgically removed 20 years ago after being involved in a motor vehicle collision. He has had no recent travel outside of the United States, and he is up to date on all immunizations.
On physical examination, temperature is 39.6 °C (103.3 °F), blood pressure is 88/42 mm Hg, pulse rate is 135/min, respiration rate is 28/min, and oxygen saturation is 90% with the patient receiving 4 L/min of oxygen via a nasal cannula. Lethargy, scleral icterus, jaundiced skin, hepatomegaly, and lower extremity petechiae are noted.
Laboratory studies:
| Haptoglobin | <8 mg/dL (80 mg/L) |
| Hematocrit | 25% |
| Leukocyte count | 4500/µL (4.5 × 109/L) |
| Platelet count | 109,000/µL (109 × 109/L) |
| Bilirubin, total | 3.9 mg/dL (66.7 µmol/L) |
| Creatinine | 1.0 mg/dL (88.4 µmol/L) |
| Lactate dehydrogenase | 909 U/L |
A blood smear from this patient is most likely to show which of the following abnormalities?
A. Cytoplasmic morulae in leukocytes
B. Intraerythrocytic banana-shaped gametocytes
C. Intraerythrocytic tetrad forms
D. Intraneutrophilic gram-positive diplococci
E. Schistocytes
Answer and critique
The correct answer is C. Intraerythrocytic tetrad forms. This item is Question 62 in MKSAP 18's Infectious Disease section.
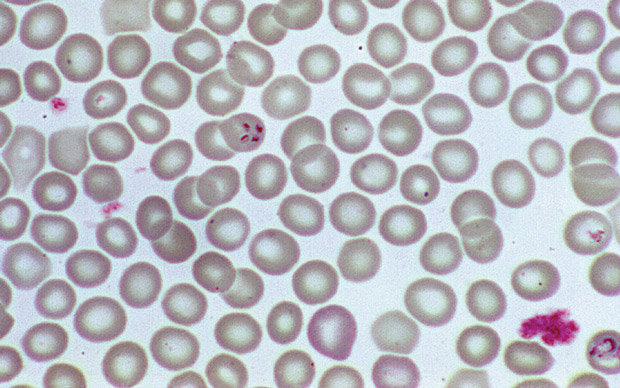
This patient's blood smear is most likely to show intraerythrocytic tetrad forms. He has a life-threatening illness characterized by fever and hemolysis and has no spleen. Given his residence in the northeastern United States and his outdoor vocation, severe babesiosis is likely. Babesia species are transmitted by the same tick that causes Lyme disease; infection also can be acquired through transfusion of infected erythrocytes outside of the endemic region. Asplenia is a major risk factor for fulminant Babesia infection, as is older age, HIV infection, or other immunocompromising conditions. Clinical manifestations are variable, with most relating to severe hemolytic anemia. Infection can be diagnosed by visualization of intraerythrocytic parasites, which appear as either ring forms or tetrads, with the latter often described as having the Maltese cross appearance shown. Complications, including acute respiratory distress syndrome, disseminated intravascular coagulation, heart failure, kidney failure, and coma, are associated with severe anemia (hematocrit level <30%) and parasitemia (exceeding 10%) and are indications for exchange transfusion.
Morulae, basophilic inclusion bodies composed of clusters of bacteria, can be seen in the cytoplasm of monocytes and neutrophils of patients with ehrlichiosis and anaplasmacytosis, respectively. These tick-borne infections cause fever, leukopenia, and thrombocytopenia but are not associated with hemolytic anemia.
Both malaria and babesiosis cause a hemolytic anemia and may present with ring-shaped parasitic inclusions inside erythrocytes. However, banana-shaped gametocytes are seen only with Plasmodium falciparum malaria, and the absence of a compatible travel history excludes this diagnosis.
Asplenic patients are at risk for overwhelming pneumococcal sepsis with a high bacterial burden; gram-positive diplococci may be visualized inside neutrophils on buffy-coat stain. Although leukopenia and thrombocytopenia are common with fulminant infection, hemolytic anemia is not a feature of pneumococcal sepsis.
Schistocytes are a manifestation of microangiopathic hemolytic anemia caused by a thrombotic microangiopathy (TMA), such as hemolytic uremic syndrome or thrombotic thrombocytopenic purpura. Although both these syndromes can cause fever, hemolysis, and thrombocytopenia, the absence of acute kidney injury in this patient excludes a TMA.
Key Point
- Babesiosis can be diagnosed by visualization of intraerythrocytic parasites in a ring or tetrad form on a blood smear.





