MKSAP Quiz: Discussing results of imaging
A 42-year-old man comes to the office to discuss results of imaging studies, which were ordered because of a change in his pattern of chronic migraine. Headache episodes have now improved.
On physical examination, temperature is normal, blood pressure is 110/80 mm Hg, pulse rate is 80/min, and respiration rate is 16/min. All other findings from the general physical and neurologic examinations are normal.
Laboratory studies:
| Hemoglobin | 10.5 g/dL (105 g/L) |
| Platelet count | 21,000/µL (21 × 109/L) |
| Alanine aminotransferase | 480 U/L |
| Aspartate aminotransferase | 600 U/L |
| Creatinine | 1.2 mg/dL (106.1 µmol/L) |
| Urinalysis | 3+ protein |
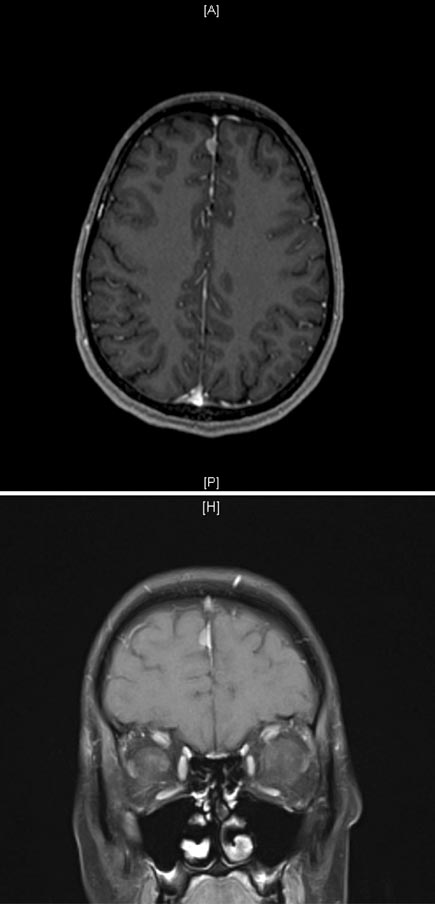
A noncontrast CT scan of the head shows a hyperintense extra-axial lesion located between the frontal lobes (parafalcine), which is confirmed by the axial (left) and coronal (right) MRIs shown.
Which of the following is the most appropriate next step in management?
A. Lumbar puncture
B. Radiation therapy
C. Repeat MRI in 3 to 6 months
D. Surgical resection
Answer and critique
The correct answer is C: Repeat MRI in 3 to 6 months. This question can be found in MKSAP 17 in the Neurology section, item 5.
Repeat MRI in 3 to 6 months is the most appropriate next step in management. The radiographic features associated with this patient are most consistent with a meningioma, which may be unrelated to his previous headaches, given the tumor's small size and lack of other symptoms. Meningiomas are benign tumors that arise from the meningeal coverings of the brain. They are the most common extra-axial (not in the brain parenchyma) intracranial lesion in adults. Meningiomas are typically slow-growing tumors, and clinical signs tend to be subtle. They also are often discovered incidentally, as in this patient. Meningiomas have characteristic imaging features, including intense homogeneous contrast enhancement (“lightbulb sign”), areas of calcification, and a dural tail, which is thickening of the dura adjacent to the mass. Patients with small, asymptomatic meningiomas without evidence of invasion of other intracranial structures and without surrounding edema are usually followed clinically and radiographically. Meningiomas should be monitored for growth, with a first follow-up scan performed 3 to 6 months after they are identified.
Lumbar puncture is not indicated in this patient whose imaging findings are characteristic of a meningioma. Lumbar puncture may be indicated in patients with suspicious imaging findings (such as partial enhancement or ring enhancement) suggestive of an infectious or inflammatory process. Lumbar puncture is only appropriate in these patients if they also have evidence of increased intracranial pressure, such as papilledema.
Patients with symptomatic tumors, tumors that invade surrounding parenchyma, or tumors that grow over time may be considered for surgery and/or radiation therapy. If intervention is indicated, surgical intervention is usually the first-line therapy, followed by radiation for higher grade tumors or tumors that could not be resected completely. These treatments are not appropriate at this time in this patient who has none of these indications.
Key Point
- Meningiomas have characteristic imaging features, including intense homogeneous contrast enhancement (“lightbulb sign”) and a dural tail.