MKSAP Quiz: Fever, chills, rash in the ED
A 55-year-old man is evaluated in the emergency department after experiencing fever and chills yesterday evening and bilateral arm pain and a rash on the upper extremities upon awakening this morning. The patient ate raw oysters from the Gulf Coast 3 nights ago. He was recently diagnosed with hemochromatosis.
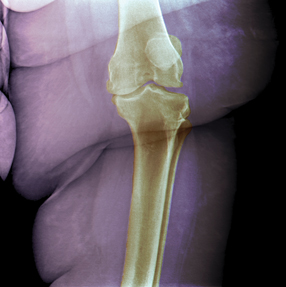
On physical examination, the patient is ill appearing. Temperature is 39.1°C (102.4°F), blood pressure is 85/50 mm Hg, pulse rate is 130/min, and respiration rate is 28/min. Skin findings of the upper extremity are shown.

Cardiopulmonary examination findings are normal. On abdominal examination, there is shifting dullness and no guarding or rebound. No signs of meningeal irritation are present.
Laboratory studies are as follows:
| Leukocyte count: | 28,000/µL (28 × 109/L) with 93% neutrophils, 6% lymphocytes, and 1% monocytes |
| Ferritin: | 1000 ng/mL (1000 µg/L) |
| Albumin: | 2.3 g/dL (23 g/L) |
| Aspartate aminotransferase: | 145 U/L |
| Alanine aminotransferase: | 100 U/L |
The peripheral blood smear is normal.
Which of the following pathogens is most likely causing this patient's current findings?
A. Babesia microti
B. Capnocytophaga canimorsus
C. Rickettsia rickettsii
D. Vibrio vulnificus
Answer and critique
The correct answer is D: Vibrio vulnificus. This question can be found in MKSAP 16 in the Infectious Disease section, item 16.
This patient most likely has necrotizing fasciitis secondary to Vibrio vulnificus infection. He has hemochromatosis with evidence of portal hypertension (ascites). V. vulnificus infection should always be considered in a patient with liver disease who presents with sepsis and cutaneous manifestations of hemorrhagic bullae after possible exposure to this waterborne, gram-negative rod. Increased iron availability has been shown to enhance the virulence and growth of V. vulnificus, which perhaps explains why patients with hemochromatosis are more likely to develop infection in addition to their having the decreased opsonization and serum bactericidal activity found in patients with liver disease. Septicemia occurs after ingestion of raw or undercooked shellfish, usually oysters. Patients may also develop wound-associated V. vulnificus infection when the pathogen is inoculated through traumatized skin. This organism thrives in warm brackish or salt water, such as the Gulf of Mexico, and most infections occur during the summer months, when seawater temperatures facilitate its growth.
Babesia microti is the pathogen responsible for babesiosis, a tick-associated infection that occurs in the coastal northeastern and upper midwestern United States. Flu-like symptoms develop about 1 week after tick exposure, and the diagnosis is typically established by evaluation of a peripheral blood smear that shows intraerythrocytic parasites. Rash is not a typical feature of babesiosis. Patients with decreased splenic function are more likely to develop serious complications.
Capnocytophaga canimorsus is a gram-negative rod that can cause cellulitis and overwhelming sepsis in patients with decreased splenic function who have been bitten by a dog or cat.
Rickettsia rickettsii is a tick-associated pathogen responsible for Rocky Mountain spotted fever (RMSF). Although liver chemistry studies can be abnormal in patients with both RMSF and V. vulnificus infection, the rash in RMSF characteristically begins on the palms, soles, wrists, and ankles before moving centripetally to involve the trunk. The rash is initially maculopapular but eventually becomes petechial. Aseptic meningitis may also develop. RMSF is unlikely in this patient with hemorrhagic bullae.
Key Point
- Patients with liver disease are at increased risk for developing necrotizing fasciitis secondary to Vibrio vulnificus infection after eating raw or undercooked shellfish or following exposure of traumatized skin to contaminated sea water.