MKSAP Quiz: Management after a routine exam
A 35-year-old woman undergoes routine evaluation. She has no current medical problems or history of bleeding symptoms. Her medical history is significant only for iron deficiency 3 years ago that was thought to be diet related. She takes only oral contraceptive pills.
On physical examination, vital signs are normal. Examination of the skin discloses no petechiae or ecchymoses. The remainder of the examination is normal.
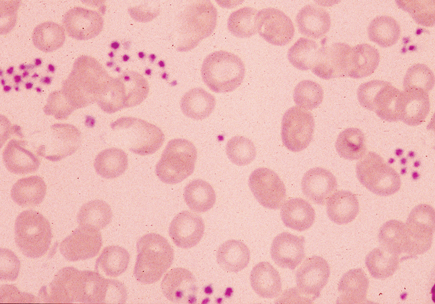
Hemoglobin is 13.5 g/dL (135 g/L), the leukocyte count is 8000/µL (8.0 × 109/L) with a normal differential, and the platelet count is 12,000/µL (12 × 109/L). A peripheral blood smear is shown.
Which of the following is the most appropriate management?
A. Initiate intravenous immune globulin
B. Initiate prednisone
C. Provide platelet transfusion
D. Repeat complete blood count in a heparin- or citrate-anticoagulated tube
Answer and critique
The correct answer is D: Repeat complete blood count in a heparin- or citrate-anticoagulated tube. This question can be found in MKSAP 16 in the Hematology and Oncology section, item 30.
The patient's peripheral blood smear shows platelet clumping, which suggests pseudothrombocytopenia. Pseudothrombocytopenia is a laboratory artifact in which platelets drawn into an ethylenediaminetetraacetic acid (EDTA)-anticoagulated test tube clump and fail to be counted accurately by the automated counter, resulting in a spuriously low platelet count. This patient's thrombocytopenia is therefore a laboratory artifact and requires no therapy. Pseudothrombocytopenia can be confirmed when the platelet count normalizes after the count is repeated in a tube containing citrate or heparin as the anticoagulant.
Immune thrombocytopenic purpura (ITP) is a relatively common cause of thrombocytopenia. The diagnosis is based on excluding other causes of thrombocytopenia, other systemic illnesses and medications. The complete blood count is generally normal except for thrombocytopenia. Pseudothrombocytopenia must be excluded as the cause for a decreased platelet count. For patients with established ITP, initial treatment includes high-dose corticosteroids. Intravenous immune globulin (IVIG) may increase very low platelet counts in patients with ITP; however, the effect is transient (days to weeks). Because this patient has another explanation for her thrombocytopenia, ITP is not confirmed, and treatment with prednisone or IVIG is not indicated.
Platelet transfusions are not indicated in patients with pseudothrombocytopenia.
Key Point
- Pseudothrombocytopenia is a laboratory artifact with no clinical sequelae, characterized by platelet clumping on the peripheral blood smear and a spuriously low platelet count.





