Spare the emergency visit for skin and soft-tissue infections
Internists can save patients the anxiety, time and expense of an emergency department visit by screening for severity of most infections, experts say. The focus should be on acuteness and the factors surrounding onset of symptoms.
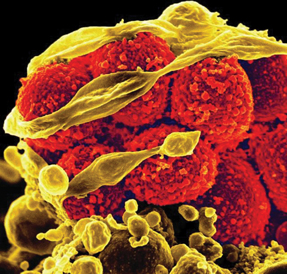
Skin and soft-tissue infections (SSTIs) account for more than 14 million outpatient visits in the U.S. each year, making them a common reason why patients seek medical care. Although methicillin-resistant Staphylococcus aureus (MRSA) grabs the lion's share of headlines, internists see patients with a plethora of conditions ranging from uncomplicated, superficial lesions to serious, potentially life-threatening deep-tissue infections.
The variety of injuries and organisms responsible for these infections presents a diagnostic challenge, but internists can save many of their patients the time and expense of a visit to the emergency department (ED) by screening for severity.
Because of the “mix and match” nature of SSTIs, questioning should begin on the telephone, when the patient first calls to make an appointment. Conditions like necrotizing fasciitis can be fatal without immediate treatment, and waiting for an office visit could prove lethal.
According to Lawrence J. Eron, MD, FACP, associate professor of medicine at the University of Hawaii's John A. Burns School of Medicine in Honolulu and coauthor of ACP's Physicians' Information and Education Resource (PIER) module on cellulitis and soft-tissue infections, several symptoms are red flags that warrant a referral to the nearest ED.
“If there is fever, rapidly spreading redness, rapid heart rate, or extraordinary pain that is disproportionate to the wound or injury, that is when you tell the patient to visit the hospital,” he said. “You don't want to be blithe about what could be flesh-eating strep or necrotizing fasciitis because they can cause serious problems in a matter of hours, including multiorgan failure.”
Likewise, internists should err on the side of caution when speaking with patients who are immunocompromised, such as those who are undergoing chemotherapy, have had a transplant, or have HIV, said Thomas Rebbecchi, MD, associate professor of emergency medicine at Cooper Medical Center in Camden, N.J.
“It's not only that they are more likely to get infections, but that they are more likely to have complications and suffer bad outcomes,” he said. “Infections should be treated more aggressively in these patients from the outset.”
The importance of history
Internists who see patients for potential SSTIs should begin by taking a thorough history of the symptoms and any events that preceded them, said Dennis L. Stevens, MD, PhD, FACP, chief of the infectious diseases section at the Veterans Administration Medical Center in Boise, Idaho, and a PIER module coauthor.
“Focus on acuteness,” he said. “How long ago did this start? Did it develop on its own or was there some complicating situation like a recent surgical procedure, an animal bite, recent trauma, wading in the Gulf of Mexico, exposure to fresh water, or travel and injury abroad?”
The answers to these questions will help pinpoint the culprit, he added. For example, cat and dog bites are associated with infection by Pasteurella multocida. Dog bites also carry the risk of infection with Capnocytophaga canimorsus. Exposure to seawater could suggest Vibrio vulnificus or Mycobacterium marinum.
The patient's overall health is another concern, as some conditions may mask infection, Dr. Stevens said.
“If the patient has neutropenia associated with chemotherapy, they may not experience the redness, swelling, and pain normally associated with infection,” he said. “Patients with diabetic neuropathy may not feel pain from developing ulcerations, which frequently act as a portal of entry for unusual organisms that may cause loss of limb.”
A significant body of research indicates that certain conditions raise the risk of infection by particular organisms. A 2008 review by researchers at McMaster University in Hamilton, Ontario, and Toronto General Hospital noted that diabetes is associated with anaerobes, gram-negative bacilli, Staphylococcus aureus, and group B streptococci; cirrhosis is associated with higher risk of Campylobacter fetus, Klebsiella pneumoniae, Escherichia coli, C. canimorsus, V. vulnificus, and various gram-negative bacilli; and neutropenia raises the risk for infection with Pseudomonas aeruginosa.
Dr. Stevens also pointed out that subcutaneous injection of black tar heroin has also been associated with a variety of Clostridium infections, including those caused by C. perfringens, C. novyi and C. sordellii. The review also noted research indicating that patients who abuse intravenous drugs are at greater risk for MRSA and infection with P. aeruginosa, while those who engage in subcutaneous drug abuse have a higher risk of infection with Eikenella corrodens.
Finally, the review said, keep in mind that some conditions have symptoms that may mimic those of SSTIs, including gout, thrombophlebitis, deep venous thrombosis, contact dermatitis, carcinoma erysipeloides and allergic reactions.
The examination
After a thorough history, the next step is the physical examination. According to guidelines published in the January 2012 Cleveland Clinic Journal of Medicine, physicians should look for several key symptoms:
- crepitus, which could indicate a gas-forming infection;
- necrosis, which may stem from group A streptococcal infections, brown recluse spider bites, or venomous snake bites;
- fluctuance, which suggests an abscess;
- purpura, which could indicate sepsis and disseminated intravascular coagulation, notably from streptococcal infection and
- bullae, which may be caused by staphylococci, V. vulnificus, or Streptococcus pyogenes.
Although many infections will enter the skin through a wound, not all portals of entry are obvious, particularly on the lower extremities, said Dr. Eron. “One that is often overlooked is cracked skin between the toes caused by athlete's foot. If you suspect streptococcal cellulitis in the legs, look between the toes,” he noted.
In addition, Dr. Stevens suggested that recurrent cellulitis also occurs at the site of the saphenous vein donor site in patients who have undergone coronary artery bypass
Yet deep-tissue infection may occur without any breaks in the skin. According to 2005 guidelines by the Infectious Diseases Society of America (IDSA) published in Clinical Infectious Diseases, in 50% of cases of severe group A streptococcal infection, there is no portal of entry.
“This can occur when strep or another organism that has colonized other areas of the body, such as the pharynx, reaches deep tissue that has been traumatized,” said Dr. Stevens. “These patients frequently have bad outcomes because they may only have a history of trauma and severe pain out of proportion to the injury, with no immediately visible symptoms.”
Whether to order laboratory tests for the sake of tailoring therapy depends on the complexity of the infection. The IDSA guidelines note that simple, localized SSTIs usually do not require testing, and blood cultures for cases of suspected cellulitis tend not to be cost-effective as they are positive in fewer than 5% of cases.
Likewise, the guidelines state that cultures of needle aspirations of inflamed skin or abscesses are “bewilderingly variable,” uncovering a culprit in only 5% to 40% of reported series for cellulitis.
Treatment
The IDSA guidelines, which will be updated later this year, provide an in-depth discussion of the appropriate antibiotics to use for various pathogens. However, several strategies can help internists more confidently diagnose and treat SSTIs.
First, consider the inflammatory response when judging a treatment's effectiveness, said Dr. Eron.
“Most skin and soft-tissue infections are caused by strep, which prompts robust inflammation,” he said. “When you start antibiotic therapy, often the erythema will expand beyond the original border for 24 hours. This is because the bacteria, though dead, are still promoting inflammation.”
He suggests using NSAIDs or other anti-inflammatories such as prednisone in conjunction with antibiotic therapy, citing a 2005 study by researchers at the University of Missouri School of Medicine and a 1997 study from Helsingborg Hospital in Sweden, which found that cellulitis resolved more quickly in patients who received anti-inflammatory treatment than in those who did not.
Dr. Stevens, however, suggested a point of caution regarding this recommendation. “NSAIDs may mask the pain, swelling and fever associated with skin and soft-tissue infections and may mislead the physician evaluating patients with SSTIs, particularly those with more severe underlying infection,” he said. In addition, he noted, NSAIDs and steroids have not been extensively studied in this population and existing research has excluded patients with severe SSTIs, diabetic patients and those younger than age 18.
Second, recurring infections involving staphylococcus bacteria may require efforts to decolonize the patient's tissues, said Dr. Eron. “It is helpful to try to eradicate a reservoir on the patient. Usually the colonization is in the groin nasopharynx, axillae and perineum,” he said.
Treatments include mupirocin ointment in the nostrils, diluted bleach baths, and washing with chlorhexidine. Persistent recolonization suggests that the patient's family or close contacts may be sources of infection. “You're better off treating the whole family when there is recurrent staph, and have them take the same precautions with diluted bleach baths and so on,” said Dr. Eron.
Third, internists should become comfortable with draining abscesses, said Dr. Rebbecchi: “It's not technically difficult, and you can save your patients the six hours they'd spend in the waiting room at the hospital.”
The caveats are size and location, he said. “Abscesses should be the size of a golf ball or smaller. If they're any larger, or if they appear on the face, groin, or neck, you should refer the patient to the ER.”
(Abscess training simulators are inexpensive and easy to make. To learn how, see ACP Internist's step-by-step teaching module, which is based on techniques presented by the Herbert S. Waxman Clinical Skills Center at ACP's annual scientific meeting.)
After starting treatment, Dr. Rebbecchi suggests that internists use modern methods of communication for follow-up. “Have the patient take a good, clear photo of the wound 24 hours later and e-mail it to you. It's a multimedia world, so why not use the same resources we use in our nonmedical lives?”
Dr. Eron encourages internists not to shy away from treating SSTIs.
“The wonderful thing about treating these is that most of them are not life-threatening emergencies,” he said. “You have a cushion that allows you to begin effective therapy even though a patient has delayed coming in to clinic for 24 hours.”
Dr. Rebbecchi agreed. “It's also not like an ongoing condition like hypertension,” he said. “You will see your patients improve in a day or two. Plus, it's hands-on medicine for you.”




