Special Focus: Diagnosing Pulmonary Embolism
Evidence-based recommendations about care.
At least 100,000 cases of pulmonary embolism (PE) occur each year in the U.S. The National Institutes of Health reports that PE is the third most common cause of death in hospitalized patients; if left untreated, about 30% of patients with PE will die within the first few hours of the event.
Correct diagnosis is critical considering that only one-third of major pulmonary emboli are diagnosed correctly before death. Approximately 26% of undiagnosed and untreated patients with pulmonary embolism will have a subsequent fatal embolic event, and another 26% will have a recurrent embolic event that can eventually be fatal.
Determining risk
Obtain a detailed history of present illness, past medical and family history, with special emphasis on predisposition to, and risk factors for, venous thromboembolism (VTE) as well as a careful physical examination. Based on initial clinical assessment, estimate a pretest clinical probability of PE before performing radiologic imaging. Consider using the following classification based on diagnostic clinical scoring systems in the literature.
Low probability:
- Symptoms incompatible with PE or compatible symptoms that can be explained by an alternative process, such as pneumonia, pneumothorax or pulmonary edema;
- No radiographic or electrocardiographic abnormalities compatible with PE (note that many PE do not lead to radiographic or ECG changes so the absence of these findings does not necessarily put someone in the low probability category), or findings that can be explained by an alternative diagnosis; or
- Absence of risk factors for venous thromboembolism.
Intermediate probability:
- Symptoms compatible with PE, but no associated radiographic or electrocardiographic findings; or
- Constellation of findings not consistent with low or high clinical probability.
High probability:
- Symptoms compatible with PE (sudden-onset dyspnea, pleuritic chest pain, tachypnea, or syncope), not explained otherwise;
- Radiographic or electrocardiographic findings compatible with PE, or widened alveolar-arterial oxygen gradient, not explained otherwise; or
- Presence of risk factors for VTE.
A decision about further diagnostic testing should be based on the pretest probability of PE. In guidelines published in the March 20, 2007 Annals of Internal Medicine, the ACP and the American Academy of Family Physicians (AAFP) recommend using validated clinical prediction rules in estimating the pretest probability of DVT and PE. The Wells Prediction rule for pulmonary embolism (see table) is validated and frequently used, although it performs best in younger patients without comorbidities or a history of VTE. Clinical judgment is needed to correctly diagnose older patients with comorbidities.
Wells Prediction Rule: The clinical probability of PE: low, 0-1; intermediate, 2-6; high greater than or equal to 7 (see Table).
Choosing the correct test based on pretest probability
The ACP/AAFP guidelines recommend considering a high-sensitivity d-dimer in appropriately selected patients with low pretest probability of DVT or pulmonary embolism. Enzyme-linked immunosorbent assay (ELISA), quantitative rapid ELISA, and advanced turbidimetric d-dimer determinations are highly sensitive assays (sensitivity 96% to 100%). However, d-dimer testing is not specific, so the test is useful primarily for ruling out a diagnosis of venous thromboembolism but not for confirming it. Thus, a negative test indicates a low likelihood of VTE.
D-dimer testing has the highest negative predictive value when used to exclude VTE in younger patients without associated comorbidity or history of VTE and who have a short duration of symptoms. However, a d-dimer test alone may not be sufficient to rule out VTE in older patients, those with associated comorbidity, and those with a long duration of symptoms.
For patients who have intermediate or high pretest probability of PE, imaging is essential. Possible tests include ventilation perfusion (V/Q) scanning, multidetector helical computed axial tomography with contrast injected according to a “pulmonary embolism protocol” (frequently referred to as CT angiography), and traditional pulmonary angiography.
There are several advantages and limitations to choosing V/Q scanning or CT angiography as an initial pulmonary imaging study to confirm the diagnosis of PE. A normal V/Q scan excludes PE and a high probability scan is diagnostic in patients with a high clinical (pretest) probability of VTE, but 40% to 70% of patients have an indeterminate (nondiagnostic) scan and require additional testing. CT angiography has increasingly been replacing V/Q scanning as the initial study for patients with suspected PE, and it is also useful as a follow-up study for patients whose initial work-up with a V/Q scan was not diagnostic. Although CT angiography has a high specificity and is therefore effective in confirming a diagnosis of PE, CT angiography alone may not be sufficiently sensitive to exclude PE in patients with a high pretest probability.
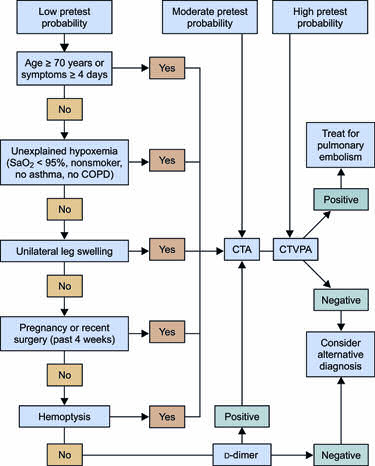
For both V/Q scanning and CT angiography, the imaging study is most useful when its results are concordant with pretest probability estimates. When imaging study results are discordant with pretest probability estimates, further diagnostic studies are indicated, such as CT angiography (if the initial study was a V/Q scan), ultrasound examination of the lower extremities, or traditional pulmonary angiography. (See Figure.)